I was going to put just the link here, but she is no longer updating this site- and i didn't want to lose it if the site goes down....sooooo
Yasmina:
Joining me here today is Dr. Diana Driscoll, optometrist and author of The Driscoll Theory, the first publication to link Ehlers-Danlos Syndrome and Postural Orthostatic Tachycardia Syndrome with abnormal intracranial pressure, suspected MCAS, vagus nerve problems, and vascular disorders. Dr. Driscoll is the president of Genetic Disease Investigators, LLC, which was set up to formally study these conditions, some peer reviewed results of which can be found on POTSCare.com. She is also a patient herself and mom to children also affected by, but now mostly recovered from these disorders and has now returned to work full time at POTS Care to help others. Dr. Diana Driscoll, thank you so much for joining me here today.
Dr. Driscoll:
Thank you Yasmina. It is wonderful to be here and thank you for having me.
Yasmina:
Dr. Driscoll is here today to share her ground-breaking findings on POTS, mast-cell activation, and the vagus nerve connection, something that I know is exciting a lot of us out there. Dr. Driscoll, would you please outline briefly for us the symptoms of POTS and when and how it affected your life and that of your children’s.
Dr. Driscoll:
Certainly. Yasmina, this has been over a decade long journey for me, as you likely know, and over time I’ve come to view POTS in two ways. First, by the definition, that is orthostatic intolerance. Patients have a rise in heart rate of over 30 beats per minute, or 40 beats per minute for kids, when going from a supine position to standing when measured over 10 minutes. Symptoms include lightheadedness, dizziness, weakness, shaking and trembling, nausea, tunnel vision, difficulty speaking, et cetera. Secondly, I view this as a syndrome. It’s a cluster of symptoms, if you will, that reaches far beyond orthostatic intolerance and includes such things as headaches, gastroparesis, constipation and IBS, extreme and chronic fatigue, difficulty breathing, hyperadrenergic tendencies, depression, sensitivities to sounds, stress, light, and movement, among other symptoms.
When I had POTS, I assumed all of these symptoms would be viewed as part of my autonomic dysfunction, but when I passed all of the autonomic testing except for the tilt table test, I came to realize that my specialist viewed these additional symptoms as basically being unrelated. That was my first hint that we were dealing with an illness that had no answers at the time. As far as my kids and I, I was completely disabled by hyperadrenergic POTS. My son, however, was a fainter and became so ill he was too sick to even be tutored, much less attend school, and my daughter had a low level of POTS that could have been easily missed by others if they weren’t looking for it. We were an interesting combination of different forms of POTS, yet we were all in the same family.
Yasmina:
Did you ever get to the root cause? Do you believe there’s more than one root cause?
Dr. Driscoll:
The root cause of POTS is tricky because there are many causes to POTS, as you know, and yet we need to locate underlying cause or causes in order to be treated effectively, but also frustrating is that over time the condition can change in presentation. One issue can lead to another, which can lead to another, and so on. We need to peel back the layers carefully to figure out what’s happening. Having said that, I strongly believe we can begin to separate folks with POTS into clusters, which helps immensely in trying to treat them. We should never try to treat all POTS patients the same way.
POTS and/or autonomic dysfunction can mimic or be the result of autoimmune, neurological, and metastatic conditions, like cancer for example. Most autonomic doctors are able to recognize and treat those conditions and this should likely begin first, but for those of us who do not fall into these categories, I call them “Idiopathic POTS”, there’s currently little help beyond symptomatic treatment that for many of us, including my kids and I, isn’t effective, at best. We need to dig deeper for Idiopathic POTS patients and that’s been my focus over the last decade. For Idiopathic POTS, I believe there are many root causes that have been missed in the past that are just starting to come to light and I’ve been on a mission to expose them.
When I initially released The Driscoll Theory, I presented the overlooked aspects of abnormal intracranial pressure, vagus nerve problems, inflammation, including but not limited to MCAS and vascular anomalies, for example. I strongly believe that we can help these Idiopathic POTS folks by considering some of these previously ignored aspects and we need to look at everything in every patient, including abnormal inflammation, chronic infection, hypermobility or connective tissue problems, vascular inflammation and anomalies, abnormalities in the immune system, and abnormal intracranial pressure. I believe that these are the most important pieces that have been missing for patients with Idiopathic POTS and are likely the root causes.
Yasmina:
I find all of this really fascinating and I wonder if I had had better doctors and if I had known what I was looking for and if I hadn’t found mast-cell activation first if I would have actually been diagnosed with POTS because when I finally looked at the symptoms after being diagnosed with MCAS, with Mast-Cell Activation Syndrome, I was really shocked to find that my symptoms corresponded almost exactly to the POTS symptoms. Things that were not really correlating to mast-cell disorder. I did still have the mast-cell activation symptoms running concurrently and I wonder what is the link between these conditions, because you have found a link and it does seem that many of us have this trifecta of conditions: the Mast-Cell Activation Syndrome, the POTS, and the EDS.
Dr. Driscoll:
Mm-hmm (affirmative), right. I don’t think you’re alone and I don’t think our doctors were being bad doctors. I think a lot of this is new to them. They really did not know. If I look back, although it makes more sense to us now, I don’t think this was common knowledge but that’s how I found answers. I have a huge advantage over most researchers in this area because I’m a patient and my kids were patients. This condition was incredibly disabling for me, as it is others, and yet most traditional testing doesn’t even hint at how affected we are. I remember telling my husband that when the doctors figure this out they will be surprised we can even survive, which hints at how very sick I was.
When so much testing comes out negative, it can be easy for some doctors to jump to anxiety or other psychosomatic diagnoses, which I believe is a tragic mistake. Instead, I had the advantage of knowing my condition wasn’t psychosomatic and I was in what I deemed to be a perfect position to try to find answers. It was a mixed blessing, but being a patient who was highly motivated to find answers was a necessary step in actually located the answers. These were answers not only for my condition and that of my kids, but for others as well. You cannot be deeply involved with patients and researchers without becoming a decent diagnostician for similar conditions, I believe.
You had asked how I found links between some of these conditions and what a great and long story. At this point you might want to sit back and relax and get a cup of tea but I’ll try to hit some of the highlights for you at least because it is a good story and I think a lot of people can relate …
Yasmina:
Share the whole story. All of it! I want to hear it all.
Dr. Driscoll:
We may need a weekend for that. There were a lot of layers that were revealed over many years that kind of hinted at what’s going on. The first thing that I noticed in my kids and I was that we had high intracranial pressure and being an eye doctor, I know the symptoms, which is headache, neck ache, nausea, tremor, light and sound sensitivity, and others, but they were getting lost in that mix of a gazillion other symptoms. Even more frustrating, the symptoms would sometimes come and go, but when I took Florinef to see if it would increase my blood volume, as many of us do with POTS, some of the symptoms just went through the roof and I was able to tell immediately that my intracranial pressure was too high. It resolved rather immediately with treatment.
Then another layer was figuring out that my kids and I were hypermobile and we were diagnosed with likely Ehlers-Danlos Syndrome. We don’t always know the gene involved so we can’t say with certainty that it’s a genetic defect, but we were told that likely the cause of our POTS was from a gradual laxity of the vessels over time because we had EDS. That didn’t sound quite right to me because there was nothing gradual about my condition, nor that of my son. Both of us developed symptoms almost overnight after viruses. I couldn’t help but notice that many others were also hypermobile, yet for most doctors were not able to find a gene [inaudible 00:10:45]for hypermobility. Until we located a gene responsible, I knew we needed to keep all possibilities open, including acquired hypermobility. Perhaps something was making our joints and even our vessels more lax and if we looked at that perhaps we could stop the decline.
Another big reveal I’ll touch on occurred with one of our first official studies. We saw 30 patients with POTS, and most had EDS or hypermobility, and 30 aged-matched normal. We took very detailed pictures of the fundus of their eyes, the back of their eyes. You see, the eye is the only place in the body we can look directly at blood vessels. We do not need to look through tissue, for example. We can magnify the image so much we can even see individual blood cells go by. We can also look directly at the optic nerve when we look into the eye. The optic nerve is often inspected when our intracranial pressure is high. I was noticing that many of us had problems with our blood vessels, everything from aneurysms, spider veins, to strokes and other clotting problems, and most of us had some neurological symptoms. I thought the eye would be a great place to start looking for answers.
I was the blinded doctor in the study, meaning I didn’t know who was a patient and who was not, but I was presented with 60 fundus images and I had to try to figure out who was a patient and who was an aged-matched normal just by looking at pictures of the back of their eye. At first, I didn’t know what to look at so I considered everything. Eventually a pattern started to emerge and I was correct in figuring out who was a patient 90% of the time and I was shocked. I saw some mild blurring around the parts of the optic nerve for some people. Some venous fibrosis or scarring in some. The vessel sizes were off in many patients. I found that often times the veins were too large and the arterials were too small, what we call an abnormal AV ratio, artery to vein ratio. Although we were calling the results normal in these exams, clearly we were missing too much and I suspected some sort of inflammatory component affecting the vessels for many patients. Then we spent a few years studying inflammation.
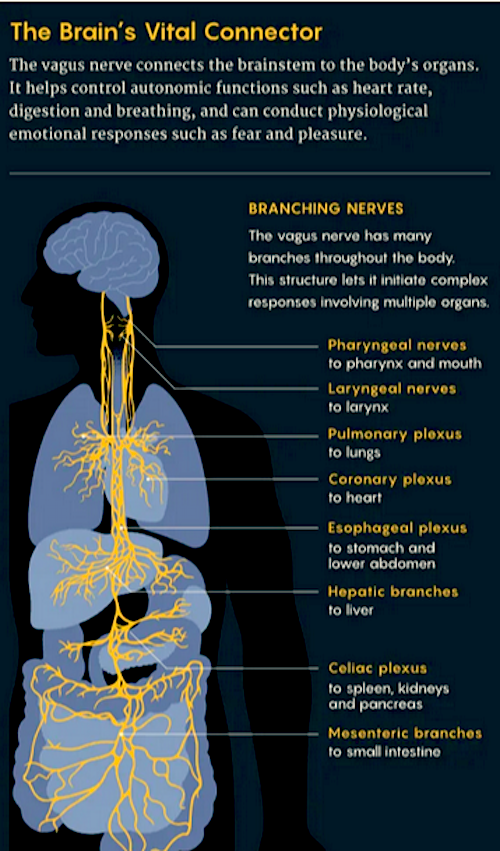
Another big reveal came when I realized that most of us had signs and symptoms of abnormal vagus nerve functioning. I think that any time the heart and the gut is affected at the same time, we need to consider the vagus nerve but nobody was really considering it at the time. The current thinking at the time was that an autoimmune condition was likely the cause of most problems with nerves involved in Idiopathic POTS. It was assumed that the receptor for the nerves was affected by these autoimmune conditions and researchers were looking hard for pure autoimmune conditions.
What helped me figure out that this wasn’t the case for me and many others was discovered by necessity. I had horrible gastroparesis that sent me to the emergency room. I hadn’t had a bowel movement in 11 days. They tried everything, as did I, to encourage a bowel movement, but nothing was working. At the time, I suspected my vagus nerve was somehow involved. When this happened, I also had pain in my lower right hand abdominal area. We ruled out most everything causing the pain and the doctors discovered that my gall bladder ejection fraction was low. I was told to have my gall bladder removed. I chose not to and here was my thinking, Yasmina. I asked the doctor if the gall bladder was filled with stones. Nope, no stones. All right, was the opening of the duct blocked or something not working? Nope, that worked fine. Was the organ inflamed or enlarged or fibrotic? Nope, it looked okay. This was sounding neurological to me and I didn’t want to remove a healthy organ if I could figure this out.
I declined gall bladder surgery and instead I found myself at the urologist’s office to rule out kidney stones because of the pain. He performed a scan where I ingested a dye and there were no stones. He was at a loss for the gastroparesis and the pain and I suspected that my ileocecal valve, the valve between the small and large intestines, was perhaps stuck in the closed position. That could be a source of that pain. He agreed at the time that that was possible and he sent me to a thoracic surgeon. He told me that not only did he not want to perform surgery, he told me that if I suspected my vagus nerve was involved never to have abdominal surgery unless it was life-threatening because surgery can cause gastroparesis because — they just cut right through the vagus nerve during surgery. Yikes.
I went home with no help, no answers, no effective medication, and no bowel movement. What we as patients are stuck in a position like that where no one is able to help us, what are we supposed to do? It was miserable. I had exhausted all the avenues I knew of to get help but that was the position I found myself in. I was miserable and the only thing I could do was to assume I was right. I remember thinking, “Okay, I’m on my own here so let’s just assume I’m right. My vagus nerve’s affected, so what can I do?”
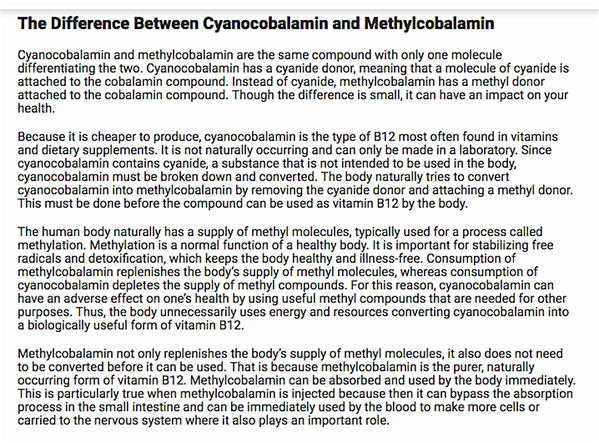
I remembered from optometry school, like a gazillion years ago, about our lecture on autonomic nerves, that the vagus nerve has 2 components: the preganglionic portion of the nerve that goes from the brain down the neck to the organ be it the heart and lungs, GI tract, or whatever, and then there’s a little gap, what we call a synapse, then there’s the postganglionic portion of the nerve, which is very, very tiny. It’s almost a part of the organ itself. I wondered if my preganglionic nerve was defunct for any reason. I was considering compression at the time. Could I possibly stimulate the postganglionic portion of that nerve and have a bowel movement? As far as I knew, my postganglionic nerve should be okay. I’ve never had surgery on that area. It should be okay. The preganglionic vagus nerve stimulates the postganglionic portion by sending a neurotransmitter, acetylcholine, across that little gap which then stimulates the organ to respond. We can’t use acetylcholine as a drug inside the body because the body immediately breaks it down. Instead, we have to use an imitator, what we call an agonist.
The vagus nerve is also special. It is a nicotinic acetylcholine nerve and a good agonist for this nerve is nicotine. I called my husband and asked him to bring home a nicotine patch. I placed the patch on the lower right hand area of my abdomen, near the ileocecal valve just kind of hoping, and about an hour later things started moving, the ileocecal valve opened and amazingly I had a normal bowel movement. Shocking, right? I couldn’t continue using a nicotine patch because nicotine activates histamine producing cells. I was on fire. It looked and felt like I was being attacked by a swarm of fire ants inside my body. It was horrible, but my response taught me two things and they’re important. First, my receptors were working fine. I did not have some rare autoimmune problem causing my gastroparesis. I did not have a receptor problem. I had a neurotransmitter problem or a problem with the preganglionic portion to my vagus nerve.
We could then stop focusing on autoimmune conditions and instead we turned to studing acetylcholine. If many of us had problems with acetylcholine, was it because we weren’t making enough, or was it breaking down somehow, or both? That’s where research went.
Another huge breakthrough came when I studied the symptom checklist that hundreds of patients with these conditions, EDS, POTS, chronic fatigue syndrome, chronic Lyme disease, and fibromyalgia sent to me through prettyill.com and many of us had some strange visual symptoms, I noticed. For example, some were bothered by viewing textured surfaces. Others had hallucinations, or where they saw insects or spiders in their visual field. [crosstalk 00:19:56] …
Yasmina:
Spiders. My God, spiders. Me.
Dr. Driscoll:
You can relate to that?
Yasmina:
Oh yes, spiders and rats from the corner of my eye and sometimes men standing in the corner.
Dr. Driscoll:
Fascinating. I hear this over and over, I’ve got to tell you, Yasmina. First, I had no idea what people were talking about until they started mentioning having snowy vision and that’s when it hit me. By studying the checklists further I saw that most patients with these chronic individual illnesses were suffering with the majority of symptoms of acute Anticholinergic Syndrome — or poisoning — and those symptoms checklists that we collected proved it. Many of us were so deficient in acetylcholine it was as if we had been poisoned by an anticholinergic drug. The symptoms would ebb and flow, however, unlike actually being poisoned. We didn’t progress to coma, seizures, and death, for example. We had such a huge number of symptoms that our physicians just weren’t recognizing this.
Likely, the reason why I was able to piece this together, looking back, was one, I was a patient experiencing some of the symptoms, right? I knew they were real. Two, I’m an eye doctor and eye doctors are very aware of these symptoms because we prescribe anticholenergics every day. The drops that your eye doctor puts in your eyes to dilate your pupils, those are anticholenergics. We learn the pharmacology, we know the presentation, so it came together for me. I think very low acetylcholine levels is a huge stumbling block for the majority of patients suffering with extreme and chronic fatigue and for many folks with idiopathic gastroparesis, too. The good thing is we can treat this fairly easily. Effective treatment was a necessary step for my own recovery and for the recovery of my children.
(This is not in the interview but I have checked the Anticholinergic Syndrome symptoms and see that I had ALL of them in the early days – Yasmina)
Yasmina:
Wow, that’s pretty amazing how you put that altogether. It’s incredible.
Dr. Driscoll:
It was a long journey.
Yasmina:
My goodness. So much of what you said just absolutely rings true for me. What I keep coming back to and what I learned from you actually was after I had gotten my mast-cell activation diagnosis, I thought, “Well, this is the end of it. You know, I’ve figured it out. It’s over.” Then I read your book and I thought, “Well, okay, interesting.” For most people Mast-Cell Activation is secondary to something else and I just thought, “Oh my goodness. Here we go again.” It was at that point I said, “You know what? I have to make my peace with things,” and just focus on just keeping my head down and doing the mediation, the yoga, the diet, and whatever. How does this all link to mast cells in your view? Could you elaborate a little bit on the mast cell activation as a secondary issue?
Dr. Driscoll:
Absolutely, because mast cells, of course, are inflammatory. The vagus nerve is the anti-inflammatory cholinergic pathway, so clearly there’s a link there. The vagus nerve also affects your immune system, which appears to be affected in many of us, if you’ve noticed. In the book, as you’d mentioned (The Driscoll Theory), I initially presented that perhaps high intracranial pressure could be related to mast cells because mast cells can be found in the choroid plexus, the part of the brain that makes cerebrospinal fluid, but since then I’ve come to view inflammation in general, I think as you have, as a possible cause of both the increased production of cerebrospinal fluid and as a potential reason for slowing its drainage, both of which could cause intracranial pressure. Since then also I’ve stepped away from viewing mast cells in isolation. The inflammatory cascade is very complex.
One component of inflammation increases other components. If mast cells are getting activated, other components of inflammation are also getting activated and we can’t ignore those. If we focus solely on treating mast cells, we risk leaving the patient with continuing inflammation and illness. We need to expand our scope to other histamine producing cells, certainly, and to the other cytokines and chemokines that they in turn activate. Unless tryptase is elevated, we can’t know that our illness is only a mast cell condition, or even primarily amast cell condition. We must keep our minds open and consider the entire inflammatory cascade to get answers.
Yasmina:
My tryptase has always been normal. Actually, better than normal.
Dr. Driscoll:
Fascinating. You’re not alone. When I first wrote the book and I was first going through this journey, similar to you, every layer I figured out I would think, “That’s it. We got it. We’re done. Corrected it.” Then another layer would kind of reveal itself. When I first corrected intracranial pressure and then noticed antihistamines were helpful, then saw vagus nerve problems, I thought I was never going to get to the end of the story. It was incredibly frustrating and I really feel for others going through that journey.
Yasmina:
You just mentioned about treating mast cells alone. Did you think we need to re-examine treatment options for POTS, mast cells, and EDS. My approach isn’t for everybody but … In fact, please, do not ever stop taking any medication you have been prescribed, but I felt that my body started healing in earnest when I came off my medications. I was on so many different medications. For all of those symptoms of the anticholinergic issue, all of those symptoms somewhat resolved on various psychiatric medications and then others made it worse. The Xanax for a decade certainly couldn’t have helped because that’s an anticholinergic.
Dr. Driscoll:
Right. Not only should we re-examine these conditions, we are re-examining them and treating accordingly. In addition to idiopathic cases of MCAS and EDS, I’d add chronic fatigue syndrome, chronic Lyme disease, presumed mitochondrial disorders where there’s no confirmation of that diagnosis with biopsies or genetic data, and even many cases of fibromyalgia, because many of these patients are suffering from similar, if not identical illnesses. For many of us, it is not the triggers that are to blame, but it’s our body’s abnormal response to these triggers that’s making us chronically ill. When we great that properly, we’re seeing dramatic improvements, even full recoveries in many patients.
You mentioned Xanax. I can tell you that it’s a Hyperandrogenic POTS patient’s godsend. I depended upon Xanax for survival yet I was able to go off it, basically cold turkey after reducing my intracranial pressure and then restoring acetylcholine. Clearly, my parasympathetic nervous system, the calming system of the body that allows us to what they call “rest and digest”, wase not working and yet the doctors instead saw my condition as an overactive sympathetic nervous system response and they were trying drugs to calm the sympathetic nervous system, which could help but it did not make me well. Looking back, it made so much more sense to me now that rather than having an overactive sympathetic, I had an underactive parasympathetic. You see how that balance is important?
Yasmina:
Mm-hmm (affirmative)
Dr. Driscoll:
Hitting the cause allowed the balance to recur. I have no doubt. There are answers for these chronic, invisible illnesses. My kids and I are living proof of that. Too often we’re not looking in the right places and too often doctors resort to psychosomatic illnesses and diagnoses in treatment, which can marginally help us. When we stay with the science, though, we can find the answers. There is so much hope for all of us and I really want to make sure people know that there’s definitely hope.
Yasmina:
That brings us to a really exciting part of the interview, which is you are going to share with us something that some of us may benefit from that you have created, a couple of new supplements that you have and that you have rather unconventionally decided not to profit from. Could you tell us a little bit about those, please?
Dr. Driscoll:
Sure, absolutely, and you mentioned not wanting to profit from them. I decided early on not to take a profit from their sale really because I didn’t want to be biased. I don’t want to even subconsciously assume that everyone needs the same thing and stop thinking deeply and critically about each and every patient presentation. We’re not done thinking about these conditions. We can’t stop now. Honestly, I don’t want to be in supplement sales and all that entails. I really want to remain in the science and the research. I want to see patients and help take us across the finish line. That’s where I want to spend my time.
As far as the supplements go, when I was trying to work through this vagus nerve problem, I tried to consider every possible reason for poor vagus nerve function, including damage to the nerve, for example from surgery or trauma, even whiplash I thought could be a cause, desensitization of the nerve for any reason, compression for example, and low functioning of the nerve for any reason, for example infection or inflammation of the nerve or from low availability of acetylcholine for any reason. I thought if we could correct any of these problems with the same thing, not matter what the cause, how powerful would that be? That was my goal.
The result was our first supplement, that’s now patented, called Parasym Plus™, the most important one of the three that we created. Parasym Plus™ boosts acetylcholine in a way that stimulates the vagus nerve while also boosting acetylcholine in our brain. When putting all of this together I had some goals for us. One, it had to cross the blood-brain barrier to help with cognition, both our brain fog and mental fatigue, which was horrible for me. Second, it had to come together very quickly in the body and be sufficient to stimulate the postganglionic portion of the vagus nerve. Third, it couldn’t ignite histamine producing cells, clearly, like nicotine can do.
Yasmina:
Thank you.
Dr. Driscoll:
Yes, right? Four, I also wanted it to work whether there was a defect in the pathway for production of acetylcholine or not and it wanted it to work no matter what the genetic defect was. I didn’t want patients to have to know their genetics, certainly. Finally, the ingredients had to fall within what the FDA already regarded as safe. I know it’s asking for a lot, but that was our goal. I had to dig deep into my old organic chemistry knowledge to put some of this together. We ran two in-house trials to check patient responses, which were dramatically positive, as it was for my kids and I. It was rather overwhelming actually. We’re calling Parasym Plus™ because it effectively stimulates the parasympathetic nervous system, the system we use for resting and digesting, plus it boosts acetylcholine levels for our brain. It was a necessary step for my kids and I to recover and to absorb nutrients normally again.
I know you talk a lot about high nutrient density in foods, which is so important. If we’re going to try to absorb those properly we have to have enough acetylcholine. We have to have proper vagus nerve function and what researchers are assuming are high level of sympathetic nervous system overload as the cause of some of the hyperandrogenic tendencies we sometime experience aren’t, but I think for many of us, that is from low functioning parasympathetic nervous system causing imbalance. The good thing about figuring that out is that we can easily treat it with Parasym Plus™.
Secondly, we added Vagus Nerve Support Soothing Digestive Aid. It contains acetic acid, apple cider vinegar, because with low vagus nerve function or any time we’re on Zantac or other medications that decrease stomach acid, we need some help in that area. It’s formulated with our sensitivities in mind. I prefer capsules over liquid in our population because I’m concerned about the inflammatory response in the esophagus to consistent exposure to drinking acetic apple cider vinegar. I do worry about that. We’ve also added ginger to it because it is so soothing to the digestive tract and we already know the science. Ginger helps increase motility in the GI tract, which is critical for many of us.
I should mention to you, too, that … I see this so often. Histamine in the GI tract can cause diarrhea and that can mask gastroparesis. I remember that I was glad I had diarrhea as a reaction because it would relieve the constipation. What a horrible way to live. I often see people start on Zantac, for example, and say, “It worked too well.” In other words, they ended up with constipation and gastroparesis. For many of these folks, the activation of histamine cells in the GI tract is merely masking the gastroparesis that is secondary to low acetylcholine and we need Parasym Plus™ for that. We can figure out all of that if we analyse that really carefully.
Then finally we added Vagus Nerve Support, Digestive Enzymes, which is helpful when you’re first getting Parasym Plus™ in place. It takes a couple of weeks to get the GI tract in top condition again, including the gall bladder and pancreas, and it supports pancreatic functioning during that time. [inaudible 00:34:45]. With inflammation we’re very sensitive to most everything, right?
Yasmina:
Mm-hmm (affirmative)
Dr. Driscoll:
This is formulated with that in mind. If you got too much protease, for example, it inflames the stomach lining. Not good for us. A pet peeve of mine is digestive enzymes where they throw in everything they can think of. In our case, less is often more. For example, many of those digestive enzymes will contain cellulase, to break down cellulose …
Yasmina:
Sorry, amylase. I didn’t quite hear that. They contain amylase? Is that what you said?
Dr. Driscoll:
No, cellulase.
Yasmina:
Cellulase.
Dr. Driscoll:
Cellulase breaks down cellulose and it sounds good, but our bodies don’t produce cellulase. Cows produce cellulase but they need a separate stomach for that. We do not want to break down cellulose because it’s a big source of fiber, which keeps our stools soft, keeps them moving along. There is more information on the site, but we tried to consider everything that our patient population needs because we’re kind of special already. That’s it in a nutshell.
Yasmina:
Wow, that’s quite a big nutshell.
Dr. Driscoll:
We’ve been working for a while, yes.
Yasmina:
Diana, I’m really excited to hear all of this. I have been taking the Parasym Plus. ™All I can report for now is that I’m not having any adverse effects, which in my world is pretty amazing!
Dr. Driscoll:
Well that’s good. That’s right. We’ll talk because if you are not terribly deficient in acetylcholine, the changes can be subtle at first and some people noticed the changes when they go off of it, over half. The best way to take it is to take 2-3 capsules first thing in the morning on an empty stomach. The body absorbs it quickly and it comes together to stimulate the vagus nerve, usually producing a bowel movement within an hour or so. In our studies, we mixed it in smoothies and it did not result in a bowel movement. So, absorption time is important.
Yasmina:
Interesting. Okay. Yes, that’s very interesting. Yes, I had that experience with NeuroProtek. I thought, “Oh, I’m just going to come off this,” and everything’s great and then I thought, “Wow, there’s a reason I take this.”
Dr. Driscoll:
Right. Sometimes that’s a decent way to figure out what’s working. We have to go through some crazy tests on our own body because we don’t necessarily have objective markers. For example, acetylcholine, we can’t measure that in the body. There is no blood test for it. Well, there is one that some researchers will try to do but acetylcholine breaks down so quickly it’s nearly impossible to do it, so we can’t rely on that. With something like anticholinergic poisoning, doctors have to recognize it by presentation because there is not a blood test. We do sometimes have to judge some of these conditions by our presentation and by our response to treatment. That’s usually effective and that’s what we have to do with some these “invisible illnesses.”
Yasmina:
We’re wrapping things up here at the moment, but before you go I would love to hear a little bit about POTS Care because it sounds like a really exciting project. People are always writing to me and asking me, “Where can I go? Where can I go for a diagnosis?” and now there is somewhere.
Dr. Driscoll:
Yes, we are so excited about this, Yasmina. This really is a dream come true. I was disabled for over 10 years and I certainly never anticipated being functional again and certainly not seeing patients full-time and helping them with POTS, but it’s very, very rewarding to be able to go through the entire journey and then help others. This is a week-long treatment approach and it doesn’t stop there though. We see patients for a solid week for a couple of reasons. It’s really the next best thing to living with the patients. I remember thinking, “If my doctors could only live with me, they would see some of the things that I’m experiencing.” Right?
Yasmina:
Indeed.
Dr. Driscoll:
I would show up at the doctor’s office and they wouldn’t necessarily see me crash afterwards or have horrible symptoms afterwards. I could pull myself together long enough for an appointment, but that was about it. We see patients for a week so we usually can catch most of their symptoms and signs. We like to see them when they’re not doing well. Also, we have a fair number of tests we want to run and we go through their medical records exhaustively from the beginning to the end. We don’t assume any diagnosis is correct. We just start at the beginning and look at everything from as many viewpoints as we can to try to get answers. We look at a lot of the reasons I discussed that we believe are getting overlooked and approach it from that way.
After they leave, we wait for all the blood work to come in. We’re in touch with them about their response to treatment and then eventually we can get a final plan for them and approach it that way. It has just been tremendous. We only see 1 or 2 patients a week. I think if we were very, very good we may be able to sometimes see 3 but I’m not counting on it because it’s very hands-on and I think that’s necessary for us. No two patients have been the exactly the same. There’s some components that are overlapping and there are some commonalities among us, but no two have been the same so I think a high level of detail and hands-on is going to be necessary. It’s been incredibly rewarding to see people respond, see people get back to their life. Some have had complete recoveries, which is awesome. Some we continue to work with to help them down that road. There are answers for these conditions. We have to look hard to find them and somebody needs to be looking. Somebody. I couldn’t find anybody to look for me so that’s what’s we’re doing here at POTS Care.
Yasmina:
That’s great to hear. I’m going to link to the POTS Care website in this post and put all your contact details. I’m really excited that you’re out there doing this work and there’s somewhere for people to come and see you. I just wanted to say thanks so much for joining me here today, Dr. Driscoll. You can find Dr. Driscoll’s genetic papers under the research section of the POTSCare.com website or find her at prettyill.com. I’m going to link to all of the supplements also in this post.
Dr. Driscoll:
Thank you so much Yasmina. I appreciate it all so much.
You can find Dr. Driscoll’s genetic papers under the research section of the POTScare.com website, or find her at prettyill.com